A number of posts from the Cardiovascular Health thread are relevant here so I’ve collected and condensed them for review. So we don’t rehash the same stuff.
ng0rge
He’s not a lipidologist but what he said didn’t contradict any lipidologist that I’ve watched. Heart disease is not caused by high LDL-C alone, you have to also consider other factors. Lipidologists agree with that. The lean mass hyper-responders, keto and low carb diet are just mentioned in passing at the end.
mccoy
I remember I listened to a stemtalk podcast with Dom D’Agostino and Ken Ford, two staunch followers and supporters of Keto diet. At one point, they discussed the issue of hi cholesterol in LMHR (they both are).
Their conclusion struck me as a ton of bricks, absolutely objective and worthy of two guys who are accustomed to reason according to logic and scientific evidence:
There is no free ride
They just acknowledged the fact that sometimes all the healthspan benefits (they experienced) come with some big detriment attached.
Also, there is no certainty that, over a long time horizon, hi Apob = CV events. There is no certainty but there is a significantly high level of probability.
AnUser
Not even once was a claim made i.e that apoB doesn’t have a real causal effect with a link to a study. I understand how low carb zealots can act now though.
adssx
It is extremely unpleasant to read this conversation. @A_User: you should start a new thread titled “Why lower is better for ApoB & LDL,”
SouthHill
I was not aware that I was advocating for any diet. Nor am I advocating that ApoB is not causal in CVD. It is my understanding that the scientific consensus is that the presence of ApoB is necessary but not sufficient to cause CVD. I am 100% on board with that. I’m also interested in how to prevent CVD in the presence of ApoB; seems like an important idea.
Virilius
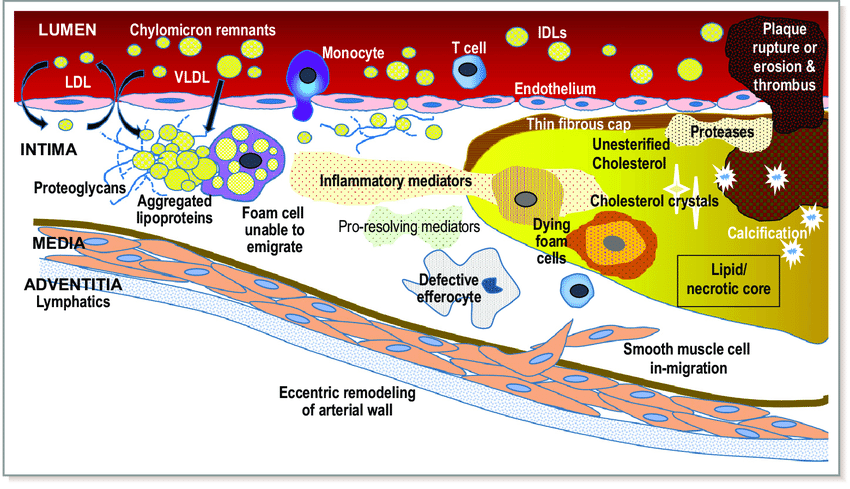
Assuming you have genetically perfect blood cell walls that NEVER let apoB particles through, you theoretically can get away with having high cholesterol values. In practice though, the combination of average cell walls and average apoB count will lead to plaque formation in nearly all cases.
JohnHemming
I think the issue with epithelial cells is senescence, if you can reduce the senescence then you don’t have to worry that much about LDL-C. However, I also think if LDL-C is high something else is probably going wrong.
ng0rge
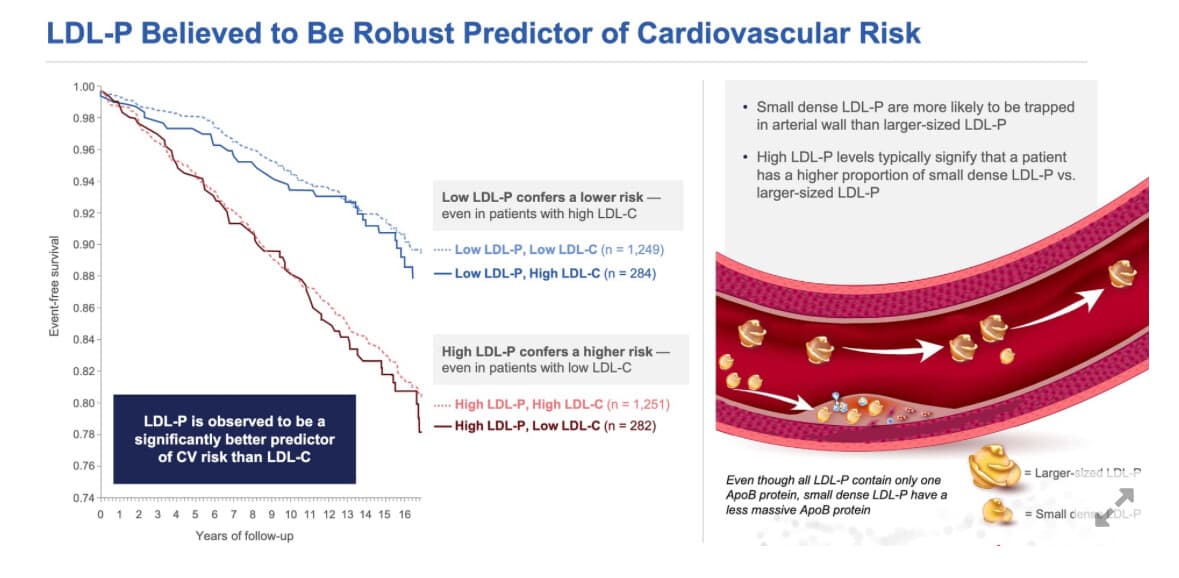
lipidology does not say that if you have high LDL-C, you will get CVD. Period. Full-Stop. Lots of people have high LDL-C and don’t get heart disease. The biggest issue and the cause of most heart disease (as pointed out in the video) is when you combine high LDL-C, or the much better measure of actual particles, ApoB, with other metabolic problems - like obesity, high blood pressure and faulty blood glucose control(and I would add inflammation). Since these are so common, it’s easy for the medical establishment to say - Just reduce your cholesterol (ApoB/LDL-C) and you reduce your chance of getting CVD - and that’s true. However, it does not mean and lipidologists are not saying, that if you are perfectly lean, healthy, getting good sleep and regular exercise, that having high LDL-C makes you unhealthy (but you should be more careful and keep a close eye on your metabolic biomarkers).
If all of your other health markers are great, high LDL-C does not have to be addressed and will only be a problem when something else goes wrong - of course that may be likely as we age. I don’t think you need superhuman genetics but you should always be careful with your diet, exercise and sleep (and stress). People on this forum are generally well positioned in terms of metabolic health so it’s not like talking to the general public. For the general public…absolutely “Lower your LDL-C!”.
Again, let me be perfectly clear, most studies are based on a representative sampling of the general public so, of course, atherosclerosis is common. But if they rounded up a group with great metabolic health, no obesity, etc. and followed them for all cause mortality just based on LDL-C, my guess would be no statistical difference. Again, not the general public and not just average metabolic health but great.
AnUser
Which lipidologists are saying that high LDL-c doesn’t make you unhealthy, in case of no other risk factors? Do you understand what causality mean? What ‘independent risk factor’ mean?
mccoy
Tom Dayspring says that there are cases with a high ApoB who do not suffer atherosclerosis and that is due to some unknown protective factor. I have been listening to hours of podcasts with him as a guest and he never hinted at the fact that in a healthy population high ApoB does not constitute a risk factor for atherosclerosis.
A few posts above I have cited a stemtalk podcast with Dom D’Agostino and Ken Ford, both staunch keto followers, both healthy guys as far as we know. D’Agostino clearly says, at 00:44, that there is a high atherogenic risk associated with an elevated cholesterol. They just accepted the trade-off with the perceived benefits. I clearly remember Ken Ford saying: “There is no free lunch!”
ng0rge
Absolutely, it’s a risk factor, and the higher your ApoB, the more risk you have of CVD. My point, again, is…You can be perfectly healthy with a high LDL-C. LDL-C ALONE does not cause heart disease.
AnUser
The low carb cult believes that ‘unknown protective factor’ is whatever they do, and they are not like the rest.
There is no heart disease without cholesterol transported through apoB containing lipoproteins. Risk factors can mediate that risk but it is enough on its own to cause disease without any risk factors, if it is increased or not.
As well as in the case of no risk factors, atherosclerosis will still continue developing…
mccoy
The first sentence is true, but you are omitting the probabilities. In the whole population, or even a healthy subgroup, what is the probability that a high LDL-C is associated to CV health (meaning: no significant atherosclerosis)?
The 2nd sentence should be reformulated, citing LDL-C as a proxy for ApoB. Then high ApoB alone according to your thesis would not cause heart disease. But this is not what Tom DAyspring and the preponderance of evidence allude to. High ApoB alone according to this eminent lipidologist is a direct cause of heart disease, since the higher the ApoB, the higher the number of collisions of such particles with the artery walls and the potential initiation of the atherosclerotic process.
I remember that the ‘safe’ threshold according to Daysping depends on other factors like blood pressure, smoke, diabetes and so on. But these just shift the threshold downwards. The threshold remains even in healthy individuals.
Dr. Thomas Dayspring
“My opinion is if you have cardiovascular risk and I’m blowing your ApoB into the stratosphere with a ketogenic diet, I want to make sure I have every other cardiovascular risk factor under control.
But the big worry nowadays, and it’s another whole lecture here is upwards of 40% of people who go on fully ketogenic diets send their ApoB level to high levels or through the roof. And boy, that becomes a whole issue, do I have to worry about that or do you not? Every other study in the history of world says you have to worry about high ApoB. Whether ketogenic induced ApoB is going to be an exception to that rule, somebody would have to do a major clinical trial to prove that.”
“Does everybody in the world who has high LDL cholesterol drop dead of a heart attack? No.”
assdx
Your guess is probably wrong.
This recent study looked at healthy people and found the same association between LDL and atherosclerosis.
What about in adults with optimal risk factors? Somewhat similar pattern.
“LDL-C, even at levels currently considered within normal range, is independently associated with the presence of subclinical coronary atherosclerosis in individuals without traditional CVRFs. Our results suggest that a stricter control of LDL-C levels may be necessary for primary prevention in individuals who are conventionally considered healthy.”
Bettywhitetest
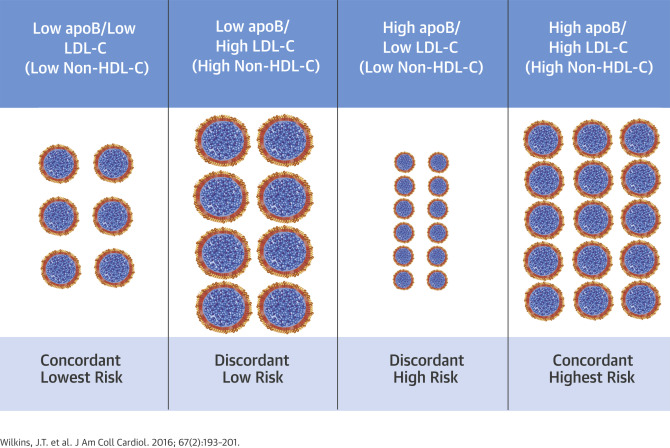
So in this study the main criteria is Non HDL levels (Total cholesterol minus HDL). Essentially ignoring Triglyceride levels if I am seeing this correctly? The conjecture of some people (like Dr. David Diamond in the video from @Bicep above) is that low Triglycerides are a “marker” for the more benign LDL particle size and hence not as indicative of heart disease in a healthy individual. Does his assumption have any merit?
I am curious also why low triglyceride levels would not be included in the Faridi et al. study as a marker of good health along with the other factors they consider such as non-diabetic, decent blood pressure etc. It seems so easy to do as most people get that measure in their lipid blood panel and could have been included in the study.
AnUser
We’ll see the goal posts continue to be moved, first it was LDL doesn’t do anything, then it was LDL doesn’t do anything for the metabolically healthy, then they will further refine the criteria to some very strict definition of healthy, eventually they will ask the analysis to only be done in low carbers.
It’s not possible to reverse atherosclerosis, correct. It’s a part of the arterial wall. Lowering LDL a lot has some regression but it’s probably not clinically significant and reason for event reduction.
Virilius
There is good evidence that high intensity statin therapy, especially when combined with other therapies such as ezetimibe and PCSK9i, can cause significant plaque regression.
Extrapolating from those results, decades of statin therapy might cause all plaque to regress eventually.
@A_User Seeing how studies consistedly show plaque regression, there must be some mechanism the body is using to get rid of soft plaque.
assdx
Yes plaque regression is possible.
------I will make one correction. William Cromwell in the video above did say that ApoB alone can cause atherosclerosis. My point is that if you look close enough, you will see another factor (SPARK) that is actually causing it.