@DeStrider, Thank you sir! I feel great.
I see no problem at all as long as you feel good
It’s wise to consider pulse pressure (PP) when looking at BP, too high or too low can mean issues.
Yours is 98/67 so your pulse pressure (pp) is 98-67 or 31.
Pulse pressure is considered low if it is less than 25% of the systolic. (For example, if the systolic pressure is 120 mmHg, then the pulse pressure would be considered low if it is less than 30 mmHg, since 30 is 25% of 120.) https://onlinelibrary.wiley.com/doi/10.1111/j.1466-7657.2011.00915.x
Yours is 98, so “too low,” an undesirable pp for you would be = <98 x 0.25 = 25 or less. It would appear that you’re comfortably above 25. Now, if your pp was narrowing over time, and moving closer to 25, then that could indicate cardiac issues such as heart failure.
Most likely as the years pass you by, your PP will slowly increase.
Bottom line: If your BP + PP have been like that for the past twenty years, and as mentioned by others that you have no s/s such as feeling dizzy when you stand up, you have good genes and likely lower cardiac risk.
FWIW
A basic overview.
Have you started indapamide @LukeMV?
I started indapamide 1.5 mg SR yesterday as telmisartan 40 mg and amlodipine 5 mg failed to lower my average SBP below 130 mmHg. However they reduced my max and although Aktiia is not well done (can’t export the data) I’m confident they increased my time in range [100-120], without any sign or symptom of hypotension (and some positive side effect of telmisartan on my mood). I’ll keep this board posted on the effect of indapamide.
No I have not. My plan was to come off the 5mg Nebivolol, which I did, and then see if my systolic blood pressure changed.
Fortunately it hasn’t, since my blood pressure regularly reads somewhere around 112/65, so I’m just sticking with the Telmisartan.
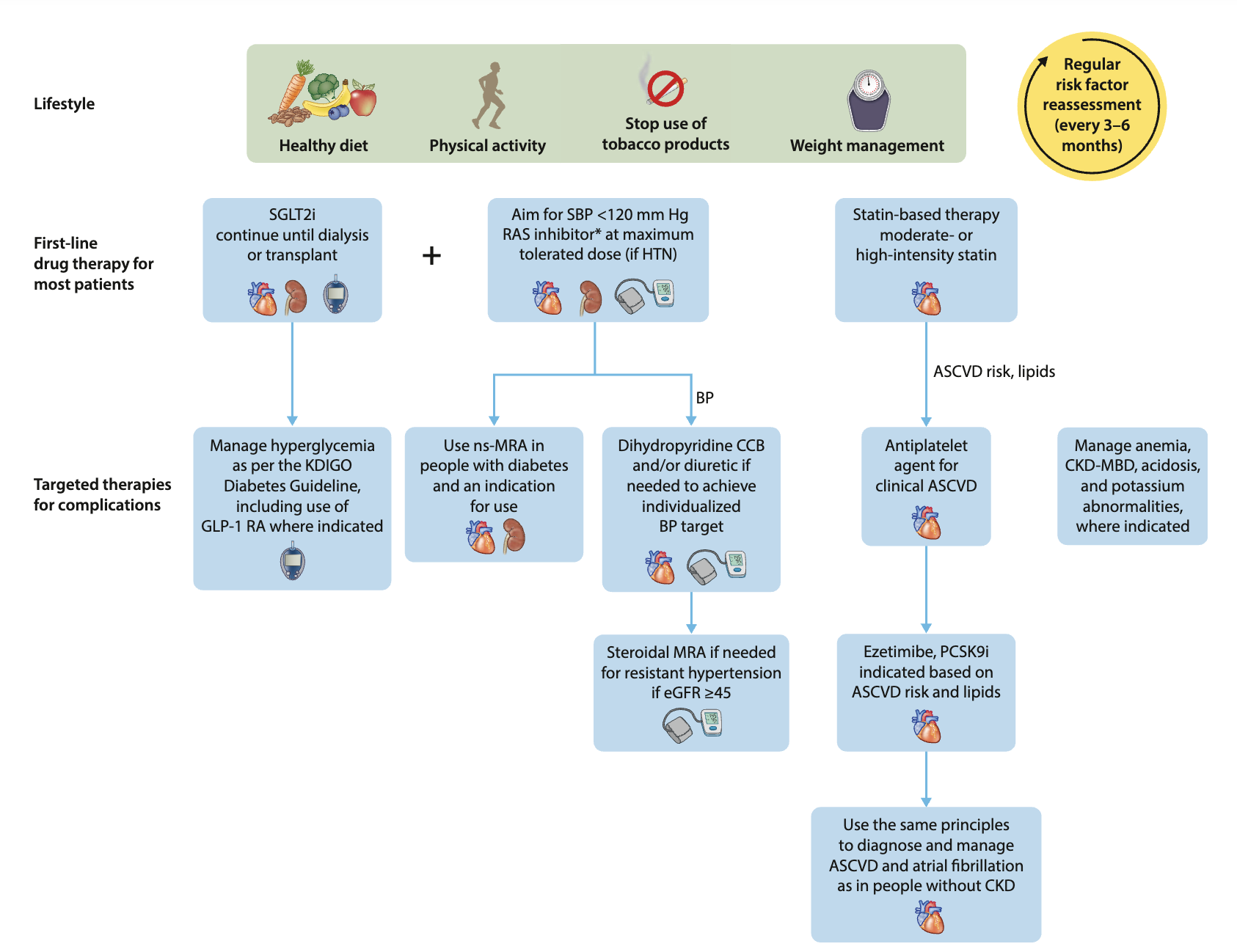
Updated international guidelines published last month: KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease
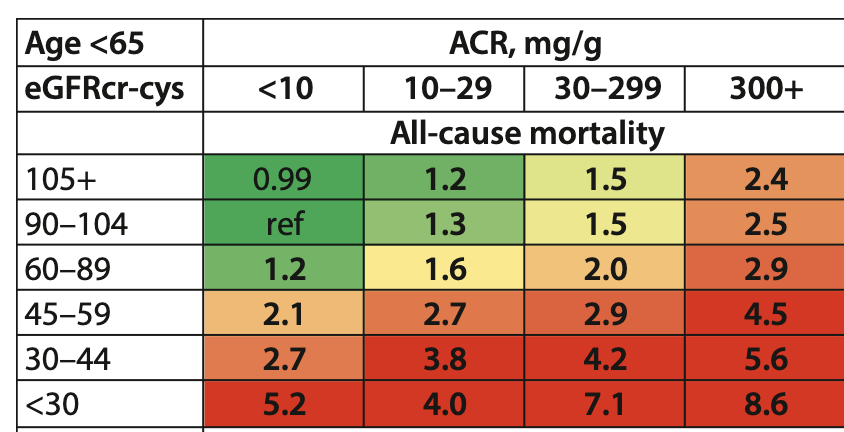
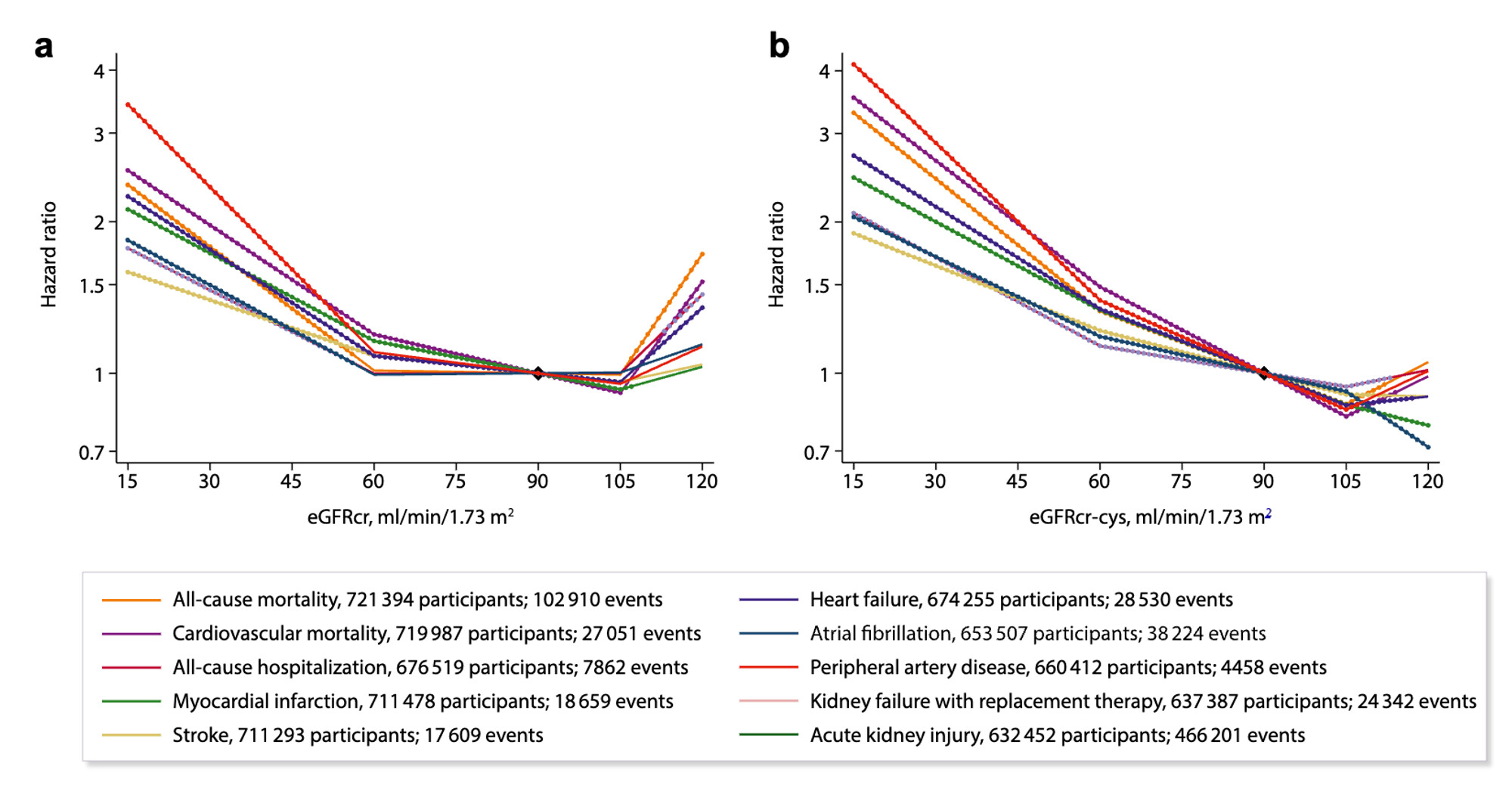
The usual suspects: SGLT2i, GLP1 RA (if needed), intensive BP control (< 120 mm Hg) with a RAS inhibitor (e.g., telmisartan, although they don’t distinguish between ACEi and ARBs), a dihydropyridine CCB (e.g., amlodipine), and a diuretic (e.g., indapamide), statin, ezetimibe, etc. These guidelines are for kidney disease. However, studies “have rather uniformly shown that the GFR declines steadily with aging, beginning at age 30–40 years, with an apparent acceleration in the rate of decline after age 65–70 years” (source) and kidney function decline is associated with increased mortality:
So is the above generalizable to everyone aged 30+?
Also, they weirdly mention rapa once in the report, but not elsewhere:
Pregnancy may pose a risk of CKD progression for people with established CKD. In addition, some recommended medications to slow or prevent CKD progression are teratogenic (such as ACEi/ARBs or mammalian target of rapamycin inhibitors) and discontinuation during pregnancy should be considered.
Is rapa renoprotective?
I actually down sized my bp cuff recently to a small when I realized my upper arm is only 22.2cm. I’m consistently getting readings of basically 100/60 +/- 1-3 points depending on when I check. Using the wrong cuff size was a rookie mistake on my part as I know better but just thought of my arms as average. ![]() Fortunately for me it doesn’t matter much but I could see where this might make a difference for some people considering medicine or having their medications adjusted.
Fortunately for me it doesn’t matter much but I could see where this might make a difference for some people considering medicine or having their medications adjusted.
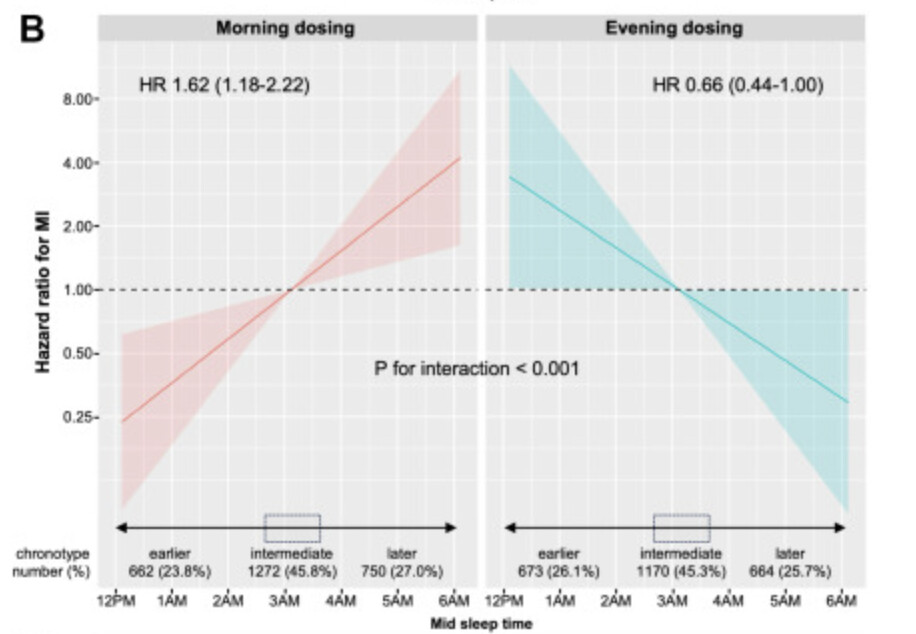
The Time You Take Blood Pressure Drugs May Lower Heart Attack Risk
Taking blood pressure medication at a time that aligns with your personal chronotype – the way your body’s circadian rhythm affects when you go to sleep and get up – could help to protect the heart against the risk of heart attack, a new study shows.
Put another way, it may be beneficial for night owls to take their medication in the evening, and for early birds to take it in the morning. These timings seem to offer some protection against the risks associated with blood pressure (also known as hypertension).
Open Access Research Paper:
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00212-8/fulltext
Sometimes when you take something makes all the difference. Thanks for this info.
Which part of the paper says this?
I understand that for “nights owls” (“later chronotype”) it’s best to do in the evening:
The composite endpoint increased for later MSFsc (later chronotype) dosed in the morning but not in those dosed in the evening (hazard ratios 1.46 [95% CI 1.14–1.86] and 0.96 [95% CI 0.70–1.30] per hour of MSFsc, respectively; interaction p = 0.036). Later chronotype was associated with increased risk of hospitalisation for non-fatal MI in the morning dosing group, and reduced risk in the evening dosing group (hazard ratios 1.62 [95% CI 1.18–2.22] and 0.66 [95% CI 0.44–1.00] per hour of MSFsc, respectively; interaction p < 0.001).
But what about the hazard ratios for the opposite?
Looking at the paper again:
- “Earlier chronotypes (the proverbial “morning larks”) are individuals who rise earlier and show peak alertness in the mid-morning hours, whereas later chronotypes (“night owls”) are late risers who exhibit peak alertness later in the day, often late into the evening.”
- “TIME was a large, prospective, pragmatic, decentralised, parallel-group study which assessed, in more than 21,000 hypertensive adults in the UK who took their usual prescribed antihypertensive medications at a single time of day (excluding night shift workers), whether there are differences in major cardiovascular outcomes between those randomised to take their usual antihypertensive medications in the morning (06:00–10:00) or in the evening (20:00–00:00).”
- “Individual chronotype was quantitatively assessed using the ultra-short version of the Munich ChronoType Questionnaire (μMCTQ)33 (Figure S1, Appendix p 16).”
- “662 (23.8%) participants in the morning dosing group and 673 (26.1%) in the evening group had MSFsc >30 min before the median and were considered ‘earlier’ chronotype. 750 (27.0%) participants in the morning dosing group and 664 (25.7%) in the evening group had MSFsc >30 min after the median and were considered ‘later’ chronotype. 1272 (45.8%) participants of the morning dosing group and 1170 (45.3%) of the evening dosing group had MSFsc within 30 min of the median and were considered an ‘intermediate’ chronotype.”
- “In line with the TIME study results, we found no effect of dosing time on cardiovascular outcomes in intermediate chronotypes (∼50% of the study population).”
- “Conversely, the risk of non-fatal stroke was not influenced by the interaction of chronotype with the administration time of antihypertensives, despite our observation that later chronotypes had a higher risk of stroke compared to earlier chronotypes, both in males and females.”
I’m rather a morning person, but according to their questionnaire, I’m actually “intermediate.” So calculate your MSFsc (mid-sleep time on free days corrected for sleep debt on workdays; ChatGPT can help ![]() ) to see whether you fall in the “earlier” or “later” chronotype category.
) to see whether you fall in the “earlier” or “later” chronotype category.
Then, if you don’t have an intermediate chronotype, do you need to change your dosing schedule based on that? There’s probably no risk in doing so, so why not?
Still, I’m skeptical about the potential benefits. I’ll quote another paper: Lowering Nighttime Blood Pressure With Bedtime Dosing of Antihypertensive Medications: Controversies in Hypertension - Con Side of the Argument 2021
Why would taking BP-lowering medications, regardless of class, regardless of pharmacodynamics or pharmacokinetics, work better when taken at night? For example, enalapril, an angiotensin-converting enzyme inhibitor, and amlodipine, a calcium channel blocker, are commonly used antihypertensive agents in Spain. Enalapril has a half-life of ≈11 hours and reaches steady state in 4 days.34 Amlodipine has a half-life of ≈50 hours and reaches steady state in 1 to 2 weeks. Once at steady state, how could the timing of administration matter? In Table 3, we show the half-life of the commonest drugs used in the Hygia trial, and the data on nocturnal BP lowering with nighttime dosing from previous studies. Indeed, a comprehensive analysis of all time-of-day trials in humans showed that medications with a half-life of <8 hours were likely to have a time-of-day dosage effect, while those with a half-life of >15 hours were not. Apart from pharmacokinetic aspects, there indeed might be pharmacodynamic effects based on time-of-day. Paradoxically, however, administration of perindopril 4 mg at 9 in the morning had a more complete 24-hour BP-lowering effect than the same dose administered at 9 in the evening in a small mechanistic randomized clinical trial. A longer discussion of pharmacological aspects of time-of-day dosing in hypertension as it relates to Hygia has been made elsewhere for the interested reader. The Hygia research team has not addressed the mechanism(s) of time-of-day dosage effects of antihypertensive medications or how the effect of a drug with a ≈50-hour half-life could be influenced by timing of administration.
It turns out that the antihypertensive drugs that many people on this forum seem to use have long half-lives:
- Telmisartan: ~24h, longest acting ARB (vs 2 to 9 hours for losartan, the most used ARB)
- Amlodipine: 35–50h, longest acting CCB (vs less than 12 hours for most other CCBs)
- Indapamide SR: 14–24h (vs 6–15h for hydrochlorothiazide and just a few hours for loop diuretics and potassium-sparing diuretics). [Chlorthalidone is the longest-acting diuretic with a half-life of 40 to 60 hours.]
So, if you use one of the above drugs, is the chronotype-based dosing still relevant? The 2024 actually looked at this question, but only in a sub-study in the appendix!
The dosing time seems potentially critical to managing disease, such as hypertension, considering the short half-life of several medications used in daily practice.
This sub-study will address the following research questions: […] Are any of these effects dependent on the half-life of the antihypertensive drug?
This study is exploratory and is intended to identify hypothesis that can be tested by further research. The analyses will use an as-treated approach and the emphasis will be on parameter estimation rather than hypothesis testing.
Effects of drug half life will be explored using the entire TIME cohort.
The models will include: evening vs morning dosing (last known dosing time), adherence (fully adherent, switched dosing time but last know time same as the allocated time, switched dosing time and last known time different from the allocated time), mid-sleep time, social jetlag, self-reported chronotype and half-life of antihypertensive.
And yet… they didn’t publish the adjusted model’s results (not even in this appendix)! So, we don’t know if the findings still hold after adjusting for sex, age, smoking status, history of heart attack or stroke, number of antihypertensive drugs, and their mean half-life. That’s really intellectually dishonest, and it’s a disgrace that a paper can be published in The Lancet with only unadjusted event rates. My guess is that the adjusted model would not be statistically significant and that if you use a long-acting drug (and you should), this paper is irrelevant.
My 3 year experience measuring PWV (pulse wave velocity) with a Withings Body Cardio scale.
Best thing that dropped my BP was getting by BMI down to 23 from 32 (46lb drop in 13 months). Have reduced my BP med doses by about 30% and my BP is averaging 110/65 the past 10 months.
https://www.rapamycin.news/uploads/short-url/vCd3GLSPNHiKGhi2t8G7PPuyQtE.pdf
The youth of today seem to be aging much faster than in the past. Check your blood pressure regularly!
Source: x.com
Open Access Paper:
https://physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.16024
Dear @DrFraser, thank you for highlighting this aspect. I experimented with an 80mg dosage of telmisartan over several days, carefully monitoring my blood pressure (with 80mg, my systolic BP decreased from 130 to 115-120 during the day, and from 120 to 110 in the morning). Interestingly, I noticed an immediate and substantial improvement in skin appearance. Attempting to explain this effect:
- PPAR-γ expression: PPAR-γ is expressed in various skin cells, including keratinocytes, fibroblasts, and sebocytes.
- Skin barrier function: PPAR-γ activation enhances skin barrier function and hydration by upregulating genes involved in lipid synthesis and keratinocyte differentiation.
- Collagen production: PPAR-γ activation may influence collagen metabolism, potentially affecting skin elasticity.
An alternative pathway: telmisartan’s effects on the renin-angiotensin system may contribute to improved skin health by influencing microvascular blood flow and reducing oxidative stress.
It is clear that my experience, though interesting, is anecdotal and warrants further investigation. ![]()
Really interesting - this is new to me, as I’ve certainly looked at PPAR expression in the brain … but was unaware it was a factor in the skin.