Yes, isolated systolic hypertension (ISH) can be harder to treat: Unsolved Problem: (Isolated) Systolic Hypertension with Diastolic Blood Pressure below the Safety Margin 2020
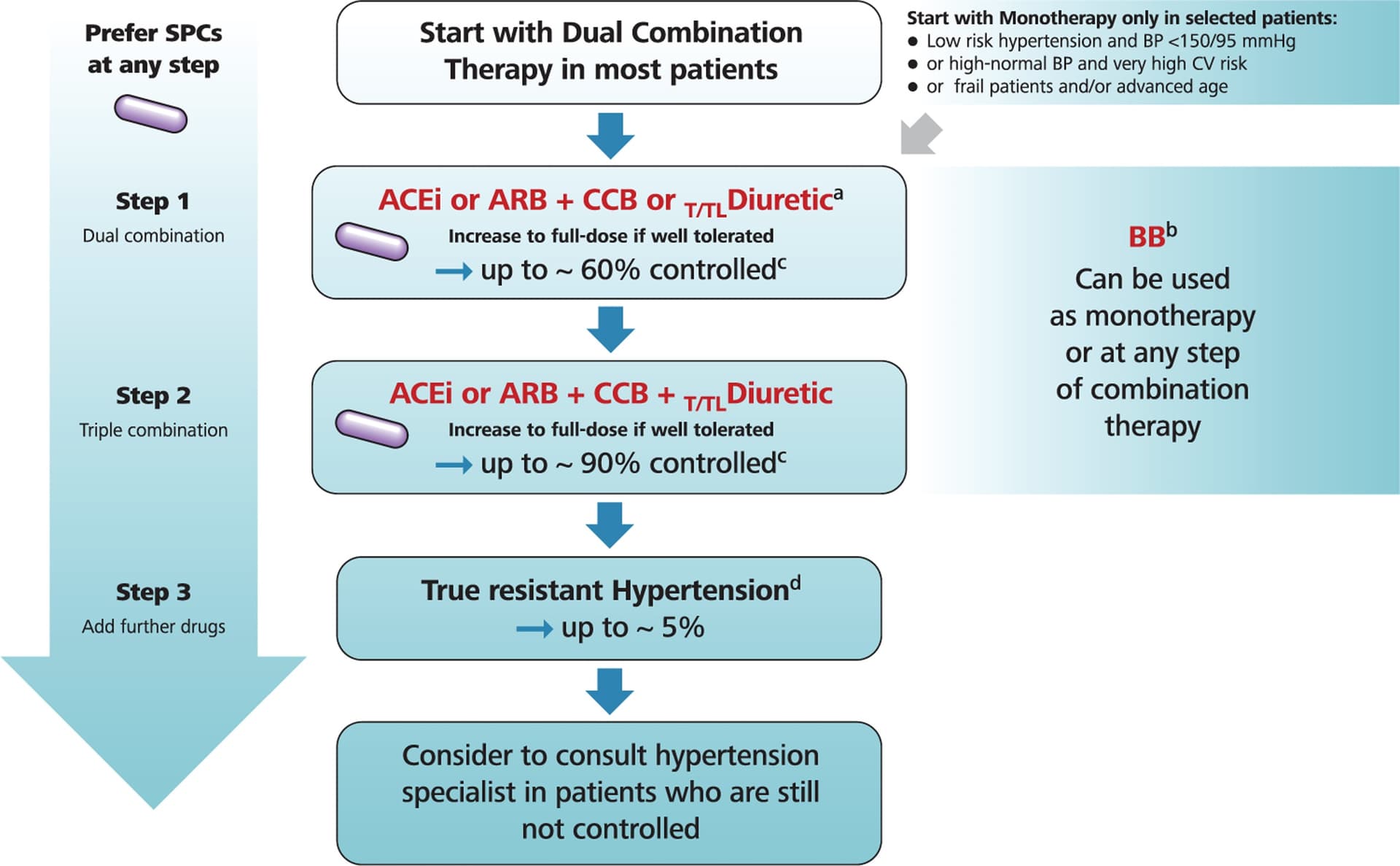
The general recommendations for (I)SH treatment mostly agree in various international and national guidelines. They differ in terms of a class of recommendations and level of evidence, but most guidelines recommend thiazide(-like) diuretics and dihydropyridine calcium-channel blockers (CCBs). The Korean Society also recommends angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers as first-line drugs for (I)SH. Experts in Canada do not recommend α-/β-blockers as the first choice of antihypertensive drug for (I)SH unless there is a compelling indication. The authors of The National Institute for Health and Care Excellence (NICE) guidelines from Great Britain recommend the same therapy as for other patients with HTN.
The 2023 European guidelines say:
Based on the data in aggregate, CCBs and Thiazide-like diuretics emerged as the drugs of choice for the management of ISH, whereas ACEis/ARBs showed less efficacy, suggesting that they should be used as first-line agents when there are compelling indications such as HF, coronary artery disease, CKD, metabolic syndrome and diabetes.
See also: Isolated Systolic Hypertension: An Update After SPRINT 2016
Drugs to Avoid: Beta-Blockers
Evidence has shown that beta-blockers have little, if any, efficacy in management of hypertension.As noted in the isolated systolic hypertension substudy of the Losartan Intervention For Endpoint reduction (LIFE-ISH) trial, atenolol was inferior to losartan for cardiovascular risk reduction.In the second Swedish Trial in Old patients with Hypertension (STOP-2) trial subgroup, the combination of diuretics and beta-blockers had the highest events for stroke, compared with ACEi and CCBs.
It’s hard to get good data on how much each antihypertensive reduces SBP and DBP as it depends on the dose but also on the individual (men and women might respond differently, there might be differences between ethnic groups as well). For thiazide-like diuretics, this paper claims that indapamide 1.5 mg SR is better than amlodipine and candesartan: Indapamide SR Versus Candesartan and Amlodipine in Hypertension: The X-CELLENT Study 2006
For the patients with isolated systolic hypertension (n = 388), the three treatments significantly reduced systolic BP, but only indapamide SR did not change diastolic BP and thus reduced pulse pressure significantly relative to placebo (P = .005). […] In patients with isolated systolic hypertension (n = 106), indapamide SR reduced 24-h systolic BP significantly more than amlodipine (P = .037), and only indapamide SR reduced 24-h pulse pressure significantly relative to placebo (P = .03).
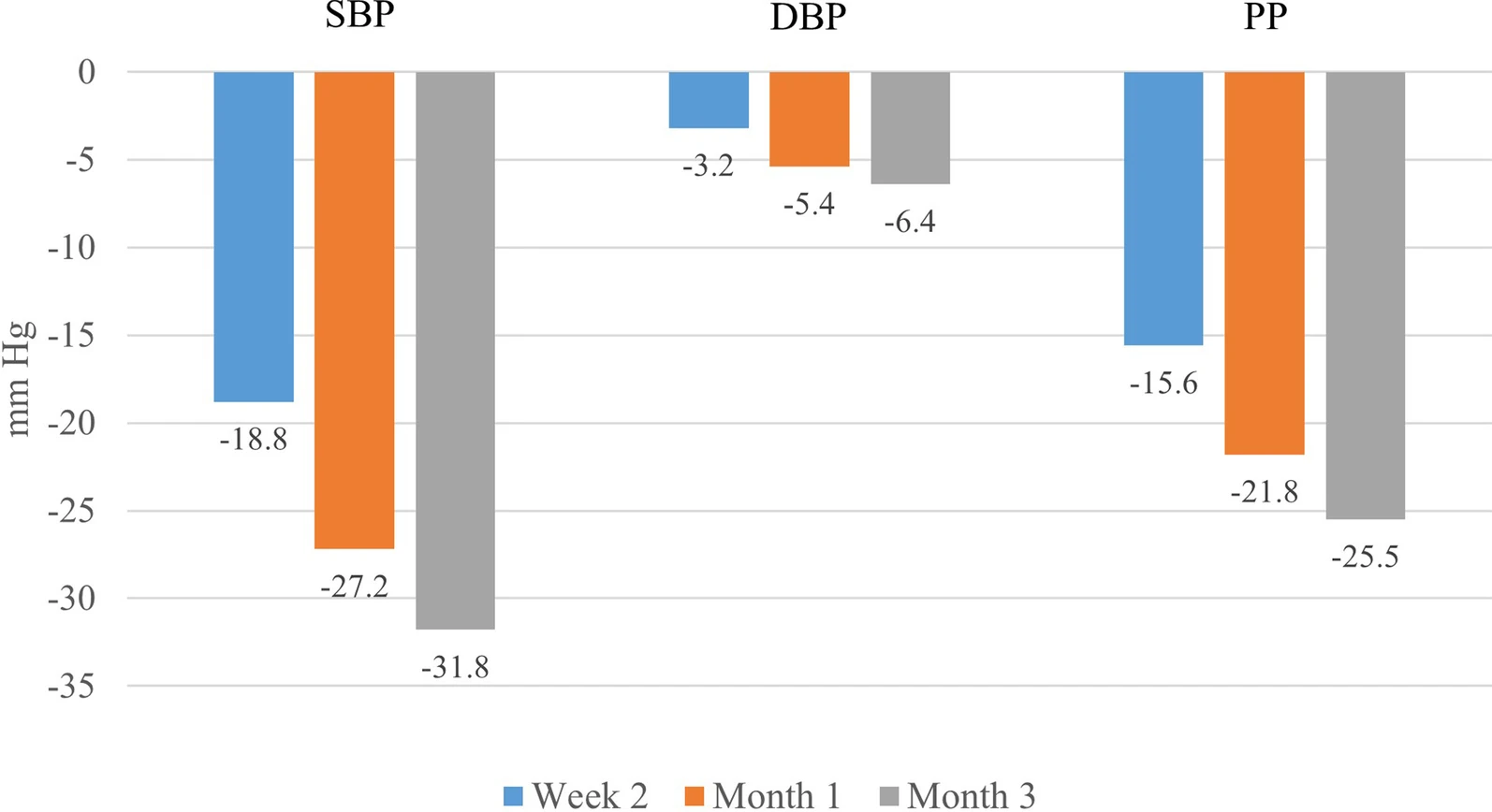
If you need even more BP lowering, another study looked at indapamide 1.5 mg SR (the sustained release version seems better than the normal indapamide 2.5 mg) + amlodipine (5 mg or 10 mg) and you can see that this combo is clearly the best at massively lowering SBP while keeping DBP in range: Effectiveness of indapamide/amlodipine single-pill combination in patients with isolated systolic hypertension: post-hoc analysis of the ARBALET study 2022
At study entry, 68.5% were prescribed indapamide/amlodipine SPC at a dose of 1.5/5 mg and 31.5% were prescribed a dose of 1.5/10 mg.
At 3 months, 60.7% of patients were receiving a dose of 1.5/5 mg, and 39.3% were receiving 1.5/10 mg
Unfortunately, they don’t give the results by dose, but I assume that 1.5/5 mg reduced DBP less than 1.5/10 mg and if that’s still too much you can use 2.5 mg amlodipine instead.
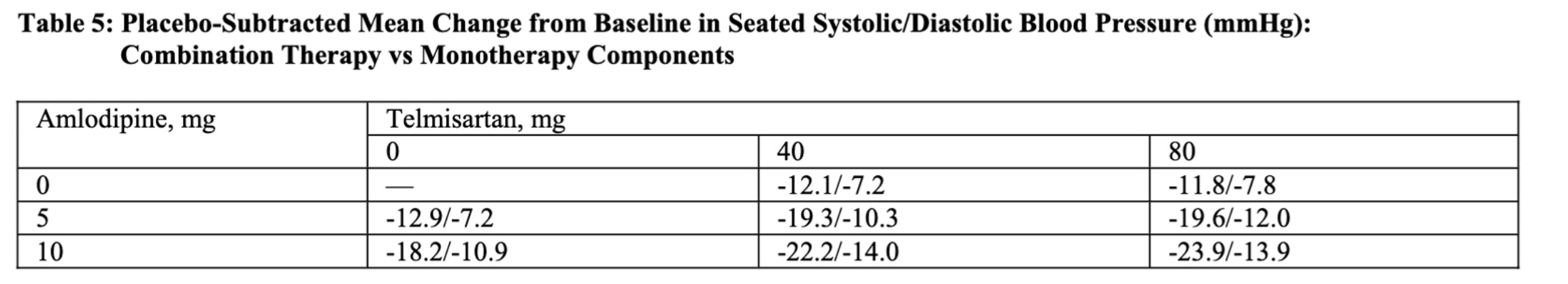
On a personal note, I’m actually considering adding indapamide 1.5 mg SR. Telmisartan 40 mg + amlodipine 2.5 mg reduced my BP only by -7/-6 mmHg to reach 127/75 (24h Aktiia), so although I’m not hypertensive anymore per Europe guidelines (<130/80), I’m still a bit higher than the US guidelines (<125/75) and I’m definitely not “optimal” (<115/75). Although it could have other benefits, pushing telmisartan to 80 mg won’t bring more SBP reduction. Increasing amlodipine to 5 mg is another option (FDA):