Wow! A year ago Lp(a) wasn’t even on the radar of most of us and our doctors, and now it is A THING! I credit Peter Attia with first alerting me to it. Got tested and found it was 40 mg/dl. Here’s some N=1 experience since that time:
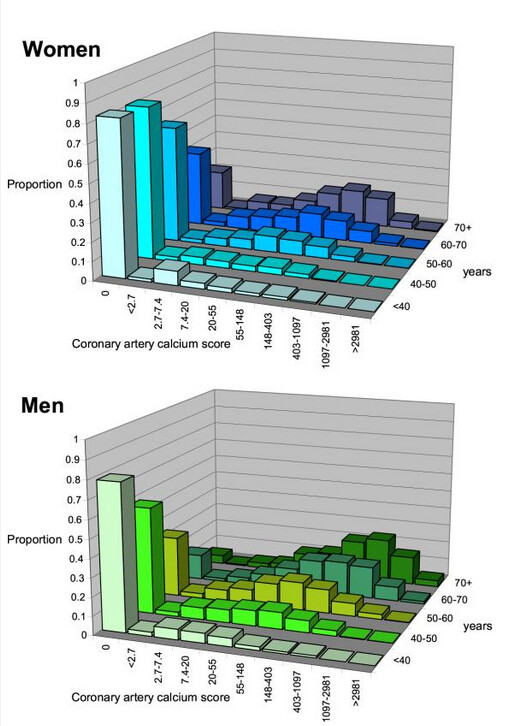
–Got a CAC score: 0.96. I am sure it would have been zero if not for having had the higher Lp(a) working on me for 74 years. Other lipids were good. Lifestyle/behavior all what they are supposed to me. I am sure my cardio situation is 100% genetic.
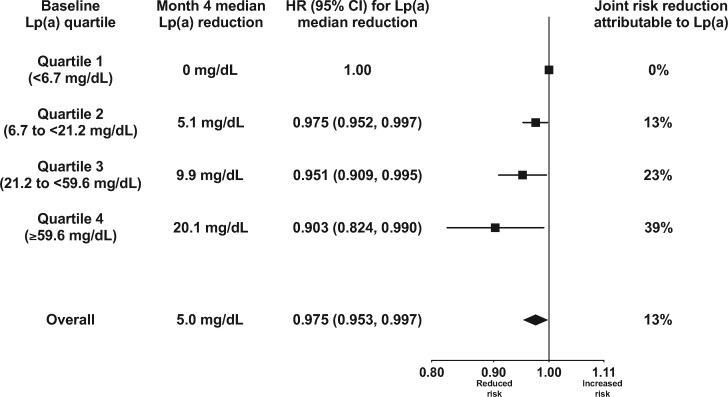
–Started Repatha which lowered Lp(a) to 29. But – glucose which had already been a little high (for years) now higher and Hb A1C into pre diabetes so asked for insulin and C peptide measurements. Which came back off the charts low. Message – if you are lucky enough to get on to Repatha – monitor your glucose and insulin. Driving down PCSK9 can impact the pancreas. The sequence by which an endogenous too-low level of PCSK9 causes the pancreas to reduce insulin is well documented. But that this can happen if you reduce exogenously with PCSK9i/Repatha --not so much. Tom Dayspring has said there are no risks to taking Repatha. Not. I am sure this is what happened to me as now numbers are starting to creep back up but still low, after having stopped the Repatha. (I do think that the Repatha might have further provoked what I feel might be a simmering LADA, which I have to get confirmed).
–Drive down inflammation – important for all health metrics, but especially for Lp(a) which is less harmful in the setting of very low overall inflammation. Depends of course on how high Lp(a) is. I exercise daily but am turning it up and swimming/using hot whirlpool three times a week instead of two. Of all the interventions, I personally have found that exercise and the heat shock proteins seem to be the most effective for reducing inflammation. (but have also stopped all alcohol and doubled down everywhere I can).
–Tell your children to get the Lp(a) checked. My son, it turns out, has it worse than I do.
–consider getting genetics tested. I did, after I discovered the Lp(a), and I found I had a 9p21 (C;C) variant: meaning homozygous for the risk allele, meaning --unusually susceptible from damage to arterial wall from inflammation and epithelial inability to repair. Don’t know it this is tied to the Lp(a) or a further additional instigator. from Promethease: " a recent study has shown that genetic variants in 9p(21) interfere with the interferon signaling pathway and effect the repair response of vascular epithelial cells to inflammation thus accelerating the pathological process of atherosclerosis leading to CAD." This single mutation puts me at 1.9x risk for cardio events.
–Surprised by all of this, as prior to the Lp(a) discovery, and subsequent genetics testing and CAD score I did not have a clue, other than some family history-- grandmother with diabetes and father died early from stroke – which I conveniently ignored as having been repeatedly told by doctors that my numbers were great and I was so healthy.
–I don’t know how to calibrate my overall risk – the contribution of (my overall very good)lifestyle versus (my abysmal) genetics for me personally – and would welcome any suggestions about this-- where to go for assessment.
–once again, N=1, YMMV, as they say. Hope this information may be helpful . . . .
PS: Rapamycin delivered a few days ago and debating whether to start . . . .even the very smallest dose.