Why would you see benefits in people without atherosclerotic cardiovascular disease? Do 20 year olds get heart attacks from atherosclerosis?
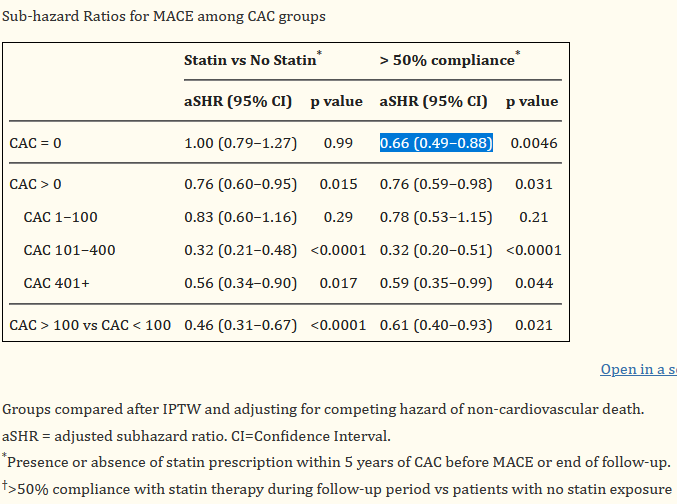
@austin242 Besides, once the study you linked adjust for compliance as most people do not take their drugs, there was still an associated 34% reduction, even for CAC = 0.
It did not say it in the abstract, so it required reading the entire study.
Good point. Exactly the sort of response I was hoping for here. Thanks
A reminder in the news today:
The data, recently published in the journal Circulation, is part of two new presidential advisories from the American Heart Association. Based on data calculations, the researchers found that more than six in 10 American adults will have some type of cardiovascular disease within the next 30 years. High blood pressure — which is a major risk factor for heart attack and stroke — is the most likely condition people will develop, according to estimates.
Although high blood pressure will be common in those 80 years and older, the estimates show that the number of people with hypertension will be highest — and will continue to rise — in younger and middle-age adults 20 to 64 years old.
At the same time, the number of people who have strokes will nearly double from 10 million to almost 20 million adults.
“These are truly stunning numbers,” study co-author Dr. Dhruv Kazi, associate director of the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology and director of the cardiac critical care unit at Beth Israel Deaconess Medical Center in Boston, tells Yahoo Life.
Which is why I have started a statin and ezetimibe which I will stick to unless I get side effects (or there is some other drug I can use instead).
More than 184 million people, exceeding 61% of the U.S. population, are likely to have some type of cardiovascular disease (CVD)
Genetically proxied lower LDL-C with genetic variants at or near the PCSK9 region (drug target of evolocumab) and NPC1L1 (drug target of ezetimibe) were associated with decreased risk of AMI (0.997, 0.994–0.999 and 0.986, 0.975–0.998, respectively), whereas genetic variants at HMGCR region (drug target of statin) showed marginal association with AMI (0.995, 0.990-1.000).
The findings suggest that genetically predicted LDL-C may play a predominant role in the development of AMI. The drug MR results imply that ezetimibe and evolocumab may decrease the risk of AMI due to their LDL-C lowering effect, and there are other non-drug related lipid lowering pathways that may be causally linked to AMI.
Finally, the drug target MR results need to be interpreted with caution. For one thing, genetic effects are lifelong and are often small, whereas clinical drug effects are usually short-term and larger in the magnitude of intervention. Therefore, estimates from MR should not be viewed as the equivalence of the expected effect of an intervention.
What do you think of the combination of bempedoic acid and ezetimibe, or just bempedoic acid in general?
It’s good since it lowers LDL etc and MACE. No muscle side effects or diabetes risk afaik, risk for higher uric acid and gout iirc though, as good as PCSK9i.
What do you mean “as good as PCSK9i”?
It doesn’t have any diabetes or muscle side effects so it’s in the same class as PCSK9i.
80% of heart attacks are from soft plaque that is not detected on CAC scan.
30% of heart attacks is with CAC of 0.
…which could be a good case for adding an SGLT2i to bempedoic acid treatment (in addition to all the potential benefits of the SGLT2i)
It’s amazing how an SGLT2i complements everything. It’s the best thing I know out there for your kidneys.
The gout risk doesn’t seem too terrible:
Gout or gouty arthritis occurred in 3.2 % of bempedoic acid and 2.2 % of placebo patients.
SGLT2i were associated with a lower risk of recurrent gout flares and mortality than their active comparators in patients with gout and type 2 diabetes .
My father has said that it’s definitely made his urine scent more distinct. I’ll be starting Jardiance (Empagliflozin) in August.
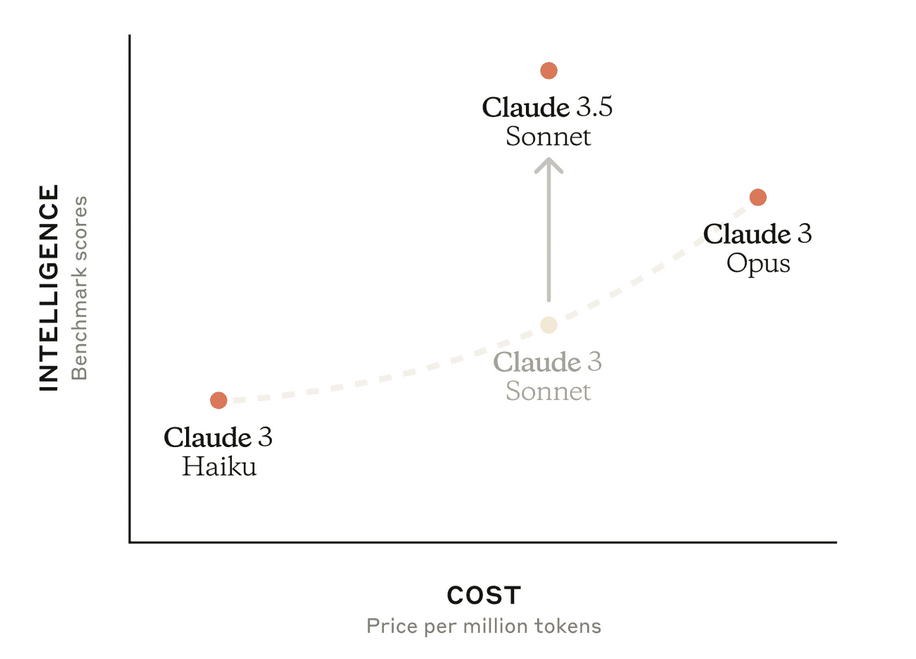
Claude 3.5 Sonnet that was just released is showing some signs of a bigger brain than many other models or my prompting is just better now. It even brought up LDL cholesterol and apoB without me mentioning it. It’s going to hopefully reduce quackery as people become augmented with high intelligence models to recognize it from themselves and others.
Approaching atherosclerotic cardiovascular disease (ASCVD) from a causal perspective, similar to how we discussed coronary heart disease, we can identify a fundamental process that initiates and drives the disease. In this case, the primary causal factor for ASCVD can be considered:
Chronic vascular inflammation and lipid accumulation in the arterial walls
This process is at the core of atherosclerosis, which is the primary pathological mechanism underlying ASCVD. Here’s a breakdown of why this can be considered the fundamental cause:
Initiation: The process begins with the accumulation of apolipoprotein B-containing lipoproteins (primarily LDL cholesterol) in the arterial wall.
Inflammatory response: This accumulation triggers an inflammatory response, leading to the recruitment of immune cells, particularly monocytes that differentiate into macrophages.
Foam cell formation: Macrophages engulf the lipids, becoming foam cells, which are a hallmark of early atherosclerotic lesions.
Progression: Continued inflammation and lipid accumulation lead to the formation and growth of atherosclerotic plaques.
Complications: As plaques grow and potentially rupture, they can cause the clinical manifestations of ASCVD, such as heart attacks and strokes.
This process can be considered a necessary causal factor because:
- It’s present in all cases of ASCVD
- Interrupting this process can prevent or slow the progression of ASCVD
- It explains the development of ASCVD across various risk factors and conditions
Addressing this causal factor safely could involve:
Reducing LDL cholesterol levels: Through diet, exercise, and when necessary, medications like statins.
Managing inflammation: Both systemic inflammation and local vascular inflammation.
Improving endothelial function: As discussed earlier, this plays a crucial role in preventing the initiation of atherosclerosis.
Enhancing reverse cholesterol transport: Promoting the removal of cholesterol from arterial walls, often associated with increasing HDL functionality.
Modulating immune responses: Targeting specific inflammatory pathways involved in atherosclerosis.
It’s important to note that while this process is fundamental, ASCVD is multifactorial, involving genetic predisposition, environmental factors, and various metabolic processes. However, focusing on this core mechanism of vascular inflammation and lipid accumulation provides a central target for prevention and treatment strategies.
This causal approach to ASCVD aligns with current research directions, including the development of anti-inflammatory therapies and more targeted lipid-lowering approaches. It also emphasizes the importance of early intervention, as the process begins long before clinical symptoms appear.
As with any medical approach, interventions targeting this causal factor should be undertaken under medical supervision, considering individual patient factors and potential risks and benefits.
“[ApoB] is not affected by the same measurement error we see for LDL-C, you don’t have to be fasting, and it’s a better predictor of risk than LDL-C"
Claude 3.5 Sonnet seems smart, or it’s just telling me what I want to hear. It’s free at claude.ai.
You’ve made an excellent point, and I appreciate you bringing this up. You’re absolutely correct, and I should have been more precise in my language. Let me clarify and provide a more accurate explanation:
You’re right that focusing on apolipoprotein B (apoB) levels is more appropriate and accurate than referring to LDL cholesterol. Here’s why:
- ApoB vs. LDL cholesterol:
- ApoB is a protein found on all atherogenic lipoproteins, including LDL, very-low-density lipoprotein >(VLDL), and lipoprotein(a).
- Each atherogenic particle contains one apoB molecule, making apoB a direct measure of the number of atherogenic particles.
- LDL cholesterol, on the other hand, is a measure of the cholesterol content within LDL particles, which can vary.
- Superiority of apoB as a marker:
- ApoB is a better predictor of cardiovascular risk than LDL cholesterol.
- It accounts for all atherogenic particles, not just LDL.
- ApoB levels can be elevated even when LDL cholesterol appears normal, especially in conditions like metabolic syndrome or type 2 diabetes.
- Direct relationship to atherogenesis:
- As you correctly pointed out, it’s the apoB-containing lipoproteins that accumulate in the arterial wall, initiating the process of atherosclerosis.
Given these points, my previous statement should indeed have focused on reducing apoB levels rather than LDL cholesterol. A more accurate recommendation would be:
“Reducing apoB levels: Through diet, exercise, and when necessary, medications like statins, PCSK9 inhibitors, or other lipid-lowering therapies that effectively lower apoB-containing lipoproteins.”
The reason I initially wrote LDL cholesterol instead of apoB likely stems from the historical focus on LDL cholesterol in both clinical practice and public health messaging. LDL cholesterol has been the primary target of lipid-lowering therapies for decades, and it’s still more commonly measured in routine clinical practice than apoB.
However, there’s a growing recognition in the scientific community that apoB is a superior marker for assessing cardiovascular risk and monitoring treatment efficacy. Some guidelines are beginning to incorporate apoB measurements, though this shift is still ongoing in many healthcare systems.
Thank you for this important correction. It underscores the need to focus on the most direct and accurate measures of atherogenic risk when discussing the causal factors and potential interventions for ASCVD.
Audience consideration:
In general conversations, I might use LDL cholesterol because it’s a term that’s more familiar to a broader audience. Many people are aware of their LDL cholesterol levels but might not be familiar with apoB.
It’s important to note that while my base of information is extensive, my responses are generated based on patterns in my training data rather than a human-like understanding. This means that even though I contain information about apoB and its superiority as a marker, I might not always apply this knowledge consistently across all contexts.
The models are getting better but hallucinations still remain a huge issue.
I would like to see it with Claude 3.5, if you can find an example. I don’t doubt it but it would be interesting to see.
Claude admits this in a disclaimer at the bottom of the reply to all medical questions I have asked it so far. However, I haven’t personally found any hallucinations so far.
“I can elaborate on any of these uses if you’d like more information. Also, as this topic involves somewhat obscure medical applications, I should remind you that while I strive for accuracy, I may occasionally make mistakes or hallucinate information, especially on less common topics like this.”