I’m not an expert but I think these are normal numbers. Hypotension is defined as <105/65 on average during daytime (nighttime: <90/50, 24h: <100/60). You’re above that. And you say you don’t even have hypotension symptoms. (Adding one more morning coffee can help increase BP if needed.)
40mg of telmisartan a day brought my numbers down to 126/79 after a week of use (hypertension is huge in my family tree). It also made me much more active which is a welcome side effect.
What was your BP before starting?
4 weeks of telmisartan 20 mg and 2 weeks of 40 mg only decreased mine from 133/79 mmHg to 125/73 (per Aktiia). So I’ve just added amlodipine 2.5 mg. Wait and see…
What do you mean by more active? I also felt something like this but I wasn’t sure it was linked to telmisartan. In Parkinson’s patients, candesartan significantly reduced apathy:
By the way, on Aktiia: it’s hard to compare to a proper cuff as it takes measure randomly. I tried to compare and there were sometimes large differences between Aktiia and my cuff (I’d say +/- 10 mmHg for SBP and +/- 5 mmHg, I didn’t do this very conscientiously…) but the daily and weekly averages were almost identical. So I trust the device to give trends. The app and the reports suck: you cannot set your own thresholds, they don’t provide proper time in range data, nor do they give pulse pressure and MAP. I now wear it 24/7, including while showering: no issue so far (I have the new waterproof model).
12X-13X / 9X.
What do you mean by more active? I also felt something like this but I wasn’t sure it was linked to telmisartan.
I seem to have much more energy and motivation without feeling restless. Stuff that I’ve procrastinated doing for months I’ve finished in days. I don’t think that’s placebo because all I expected of telmisartan was to have some additional protection from cardiovascular disease and kidney protection. I only noticed today that it might be related to telmisartan itself as that was the only medication/supplement I started recently.
In Parkinson’s patients, candesartan significantly reduced apathy:
I don’t think I have Parkinsons…
Wow impressive réduction then! You should look at your PP and MAP before/after as well.
Of course I didn’t say this but what you describe is also exactly what I felt: increased motivation, aka lower apathy. And if they were able to measure that in PD patients it might be a general “side effect” of some ARBs. There’s also an ongoing trial of ARBs for depression (but the leading researcher never answered my email…), and decreased motivation is one depressive symptom (among many others).
Hey if it helps resolve my low-grade depression as yet another benefit I’m perfectly fine with this side effect. SSRI didn’t help me at all in that regard, rather they just made me lethargic and content so I quit them after a few months.
Higher BP increases plaque formation.
@DrFraser you’ll like this: Efficacy and safety of a four-drug, quarter-dose treatment for hypertension: the QUARTET USA randomized trial 2024
Ultra-low dose quadpill of candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg vs. candesartan 8 mg for 12 weeks (and “If BP was >130/>80 mm Hg at 6 weeks in either arm, then participants received open label add-on amlodipine 5 mg.”).
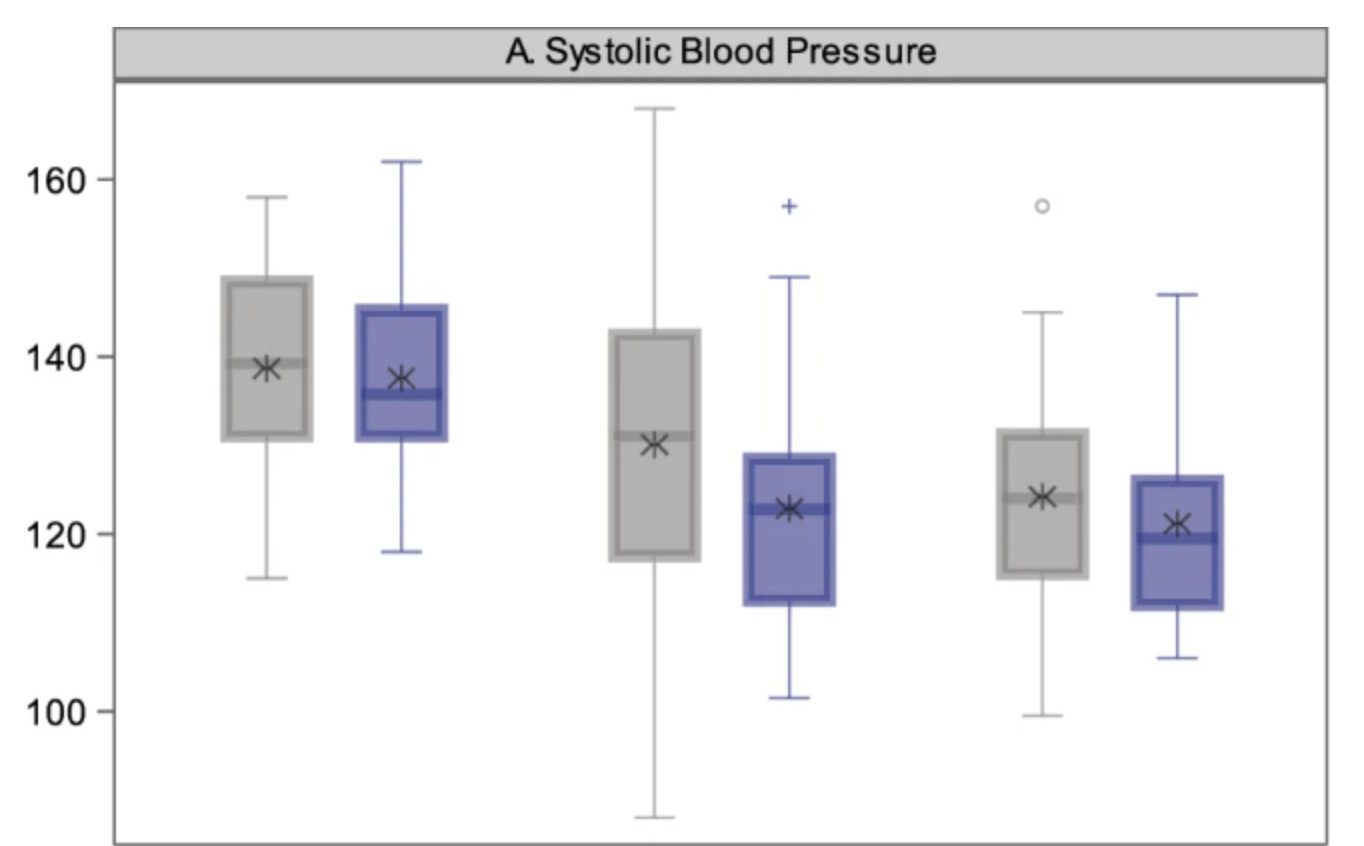
Results of the quadpill compared with candesartan 8 mg:
- SBP: −4.8 mm Hg (95% CI: −10.8, 1.3, p = 0.123)
- DBP: −4.9 mmHg (95% CI: −8.6, −1.3, p = 0.009)
I find the protocol weird; adding amlodipine 5 mg to amlodipine 1.25 mg raises the risk of edema significantly. A better protocol would have been to say “If BP >130/>80 mm Hg at 6 weeks, then double the dose”. This is probably why “A somewhat higher proportion of participants experienced one or more adverse events in the intervention arm compared with the control arm (63% versus 47%, p = 0.210).” I’m not convinced by the addition of bisoprolol either, 2.5 mg is not that low a dose: the starting dose of bisoprolol for heart failure is 1.25 mg.
It’s still interesting to see that an ultra-low dose drug combination achieves faster and better BP control than the standard dose of a single antihypertensive:
These findings were observed despite a substantially lower odds of amlodipine 5 mg add-on at six weeks in the intervention arm compared with the control arm (19% versus 53%, model estimated Odds Ratio = 0.08 [95% CI: 0.02, 0.41], p = 0.003). A higher proportion of participants achieved hypertension control defined as blood pressure <130/<80 mm Hg (66% versus 54%) in the intervention arm compared to the control arm, but the results were imprecise (model estimated Odds Ratio = 2.85 [95% CI: 0.94, 8.59], p = 0.063).
I can’t wait for the results of the GMRx2 trial (telmisartan, amlodipine, indapamide in various doses).
I agree. The general strategy with blood pressure management - at least for my patients is to gently hit multiple receptors. The rate of side effects with most pharmacologically active substances goes up as you head to maximal dose - and tends to be very low when just giving a tiny dose. Yet the benefit for most drugs is significant at low doses.
One of the substances I have some patients on for blood pressure if Hawthorne Extract - which is a fascinating extract from a berry that has multiple pharmacologic activities similar in a lot of ways to this combination they provided.
@adssx is absolutely correct - the logical approach is to double the dose of the very low dose combination.
One of the things pointed out here is just how little of an impact this had on BP. If you had a SBP of 160 mmHg - getting this down to 155 isn’t going to have you very impressed with the drug you are taking. I commonly have patients in the ER with SBP of 200 or 220 mmHg. It’s usually not an emergency to manage this as there is no short term health risk to high blood pressure (in most cases). But thinking forward as to how I’d manage them if I were their primary care physician, a combination that takes 5 mmHg off … is pretty much worthless.
Yes, it must be hard to reduce BP in these cases! In QUARTET the ultra-low quadpill decreased SBP by about 15 mmHg:
For GMRx2, they note: “The systolic BP (SBP)-lowering efficacy of GMRx2 strengths 1, 2 and 3 (Table 2) from a baseline SBP of 150 mmHg are expected to be approximately 13 mmHg, 18 mmHg and 25 mmHg, respectively.”
So how do you reduce SBP beyond 25 mmHg? I’d say:
- Lifestyle: reduce alcohol and salt intake, use potassium salt, more exercise, eat less, sleep hygiene, etc.
- Lower weight and insulin resistance (the association is impressive) with SGLT2i and GLP-1RAs
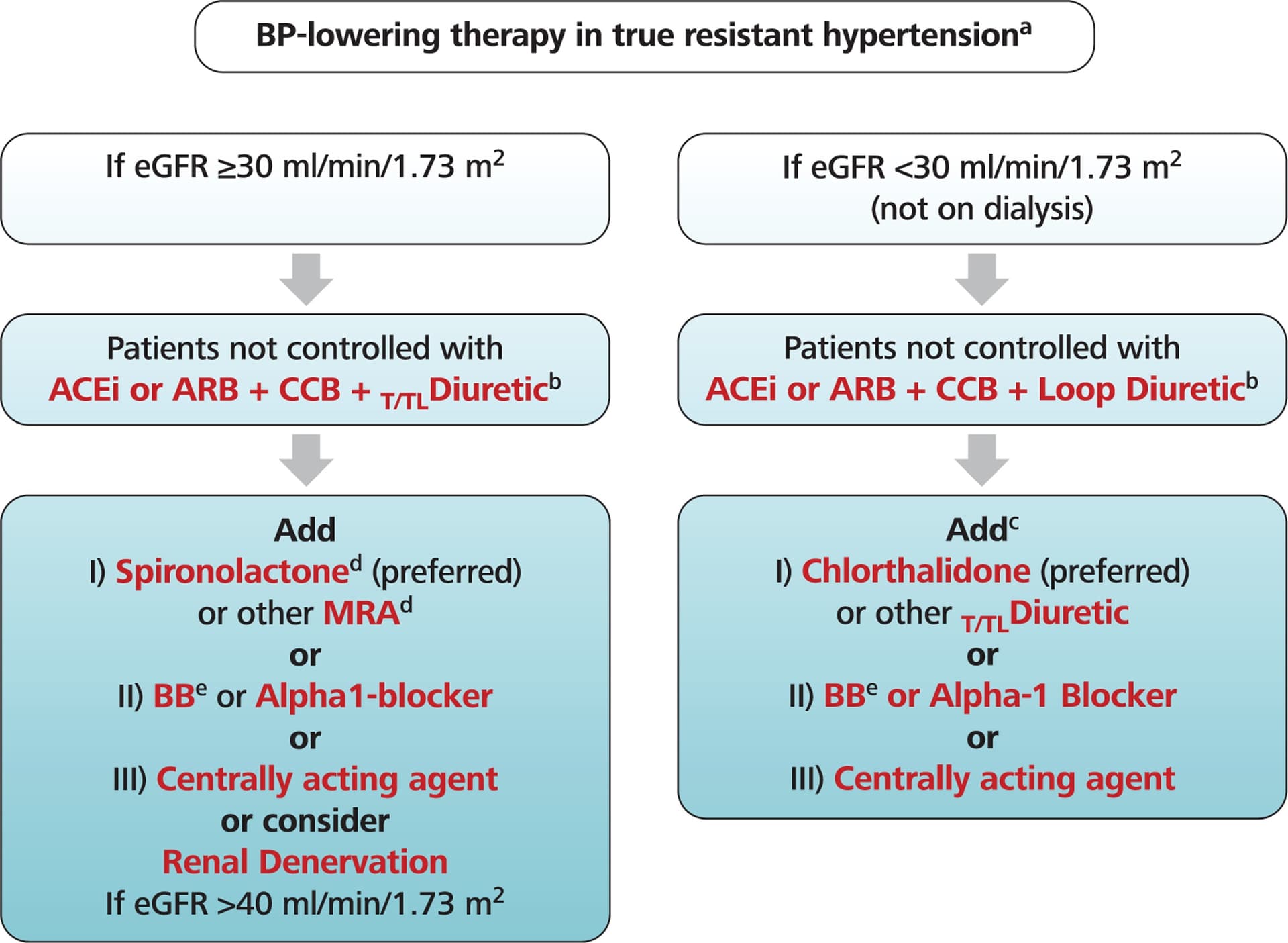
- Add another BP-lowering drug: low-dose beta blocker? spironolactone? terazosin?
These guidelines are very sensible. I think the issue is tolerability. As people get older, the tendency to have significant postural changes is a real risk for falls and loss of consciousness. There is a need for careful advice on change of position and making sure everything is doing well before just going from lying to standing and heading off. Most agents have significant risks - and when we are looking at moderate/high doses of 3-4+ classes of medications, there has to be a careful evaluation of risk/benefits.
I find that I can get most people controlled nicely with no more than 3 agents - and I do go stepwise with telmisartan, then amlodipine, then indapamide unless there is a reason to do something else. In violation of the usual approach of not pushing the dose of any drug - I will maximize telmisartan as the neuroprotection seems to occur at 80 mg but not necessarily at 40 mg.
This is an interesting area where there is nuance. Just in the same way one looks at colon, breast, prostate cancer screening and consider at what age stop doing this? It shouldn’t be the age - it should be the anticipated years of quality life potentially remaining. So if a person is expected to only live another 5 years - tightly controlling their blood pressure isn’t sensible if it risks falls and loss of consciousness - if the life expectancy might be 20 years - then managing this becomes more relevant -similarly with cancer screening.
It is complicated when having a gestalt of how long someone will live. I think I have a pretty good sense of this … as there are people who are 35 years old who are not likely to see age 40, and there are people who are 80 that I think are likely to live to 100.
Interesting. Which papers/data suggest this?
So this is an issue with PPAR-y activation which if one does a search on Pubmed you’ll see that the higher dose telmisartan seems to be important - whereas under 80 mg isn’t active.
You are much more skilled than am I finding all the references and citing them. But there are a whole lot in this space that I’ve looked through. I think if you are on telmisartan - this is a drug worth pushing to at least 80 mg before adding another drug. Also - for my patients who have risk of neurocognitive decline - if they have enough BP to allow adding this - as it usually doesn’t lower BP that much - I think it is very sensible to get them on this.
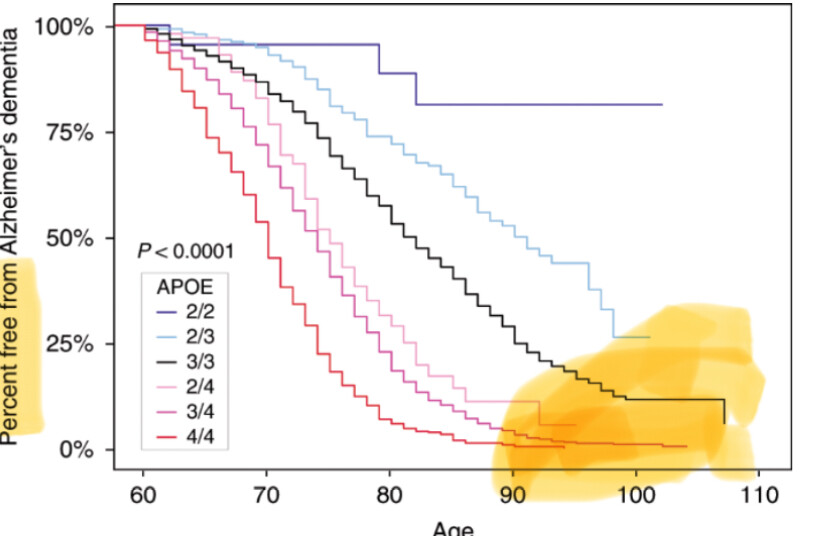
I must say the recent post by @RapAdmin showing dementia risk by ApoE status has me doubling down on the need to do everything possible to decrease risk and start as early as possible. My goal to live >100 years cognitively intact is threatened by my ApoE3/E4. I’m happy that I’m able to tolerate Telmisartan 80 mg with no seeming side effects.
Looks like you’re right!
“40 mg/day telmisartan failed to exert an appreciable clinical efficacy through PPAR-gamma activation, but showed clear effects at 80 mg”
Here is the post if anyone wants to take a look and can’t find it (was actually by me, in response to a different comment by RadAdmin):
Thanks @Neo for this great post.
I appreciate that Dr. Greger does cherry pick things a bit – but his take on ApoE is really interesting, given high prevalence on Nigeria, but low rate of AD. Here is a link to his video on this topic:
https://www.youtube.com/watch?v=zQBJScaGxJI
I think if you target all of the diseases of time early and have optimal levels, like lipids, blood pressure and blood sugar, that will have an outsized impact on Alzheimer’s dementia via compounding benefits. This should be pretty much proven at this point based on effects from short term trials that are extrapolated with MR. It probably will have a larger impact than waiting for an Alzheimer’s drug as time under treatment might be very powerful.
I believe this will end up being the case. The evidence keeps moving in that direction. It is such an interesting time to see most newer agents for T2DM having efficacy in the neurocognitive decline space. The focus of pharma with AD currently has been a failure with nothing being disease modifying - same with Parkinson’s. The clock is ticking … and for many, taking a combination of agents seems sensible. There is a risk/benefit, but it seems like the major risk for most is simply cost and coordinating care.
It would seem unlikely to me that many primary care physicians would be keen to prescribe such a combination to prevent or slow disease. This complicates things for individuals who read the literature that their primary care physicians should be reading-- who then have to obtain medications outside the usual medical system as their only option to obtain the therapies that seem sensible based on current literature.
I concur. Anyone interested in preventing NDDs (mostly AD and PD) should read this: Alzheimer’s disease risk reduction in clinical practice: a priority in the emerging field of preventive neurology | Nature Mental Health (free link)
We know the targets and the best treatments for optimal BP and blood sugar. As said in the paper, it’s not as clear for lipids, but I’m convinced newer lipid-lowering drugs (e.g., PCSK9i and CETPi) will soon be proven to be neuroprotective. Then you have the big unknown of mental health and sleep: we don’t know the best way to measure it, the targets, the treatments, etc.
This seems to be a great paper.
I’ve very much enjoyed hearing the perspectives on the senior author of the paper on the Drive over the years, including eg
- #18 – Richard Isaacson, M.D.: Alzheimer’s prevention
- Q&A on Alzheimer’s disease drug therapy with Dr. Richard Isaacson
Has anyone seen him on any more recent podcast(s)?
I like to combine hearing the thoughts of leaders like this when they are more unfiltered in addition to what they publish.